What trends do we see in delayed and deferred care since the pandemic?
Hear Insights shared by HDMS and esteemed partner Integrated Benefits Institute (IBI).
Originally presented as part of an AHIP webinar series.
Take a deeper look into mental health and also investigate how social determinants of health relate to care needs and costs.
Originally presented as part of an AHIP webinar series.
View the slides
We’re used to looking at a lot of healthcare metrics – utilization, costs, outcomes. Even just a little more data can tell us a lot more about people in context.
Check out how Plan Sponsors are surfacing measurable differences within their populations, by adding just a little more data into their analytics.
See some examples See a webinar
We’ll help you get started on measuring how healthcare needs and patterns change across different subpopulations at your organization.
Amplify analytics with SDoH enrichment. This helps reveal health inequities.
Learn more
See how easy it is to look at how social determinants of health influence your population. Find where inequities exist and track progress of program efforts.
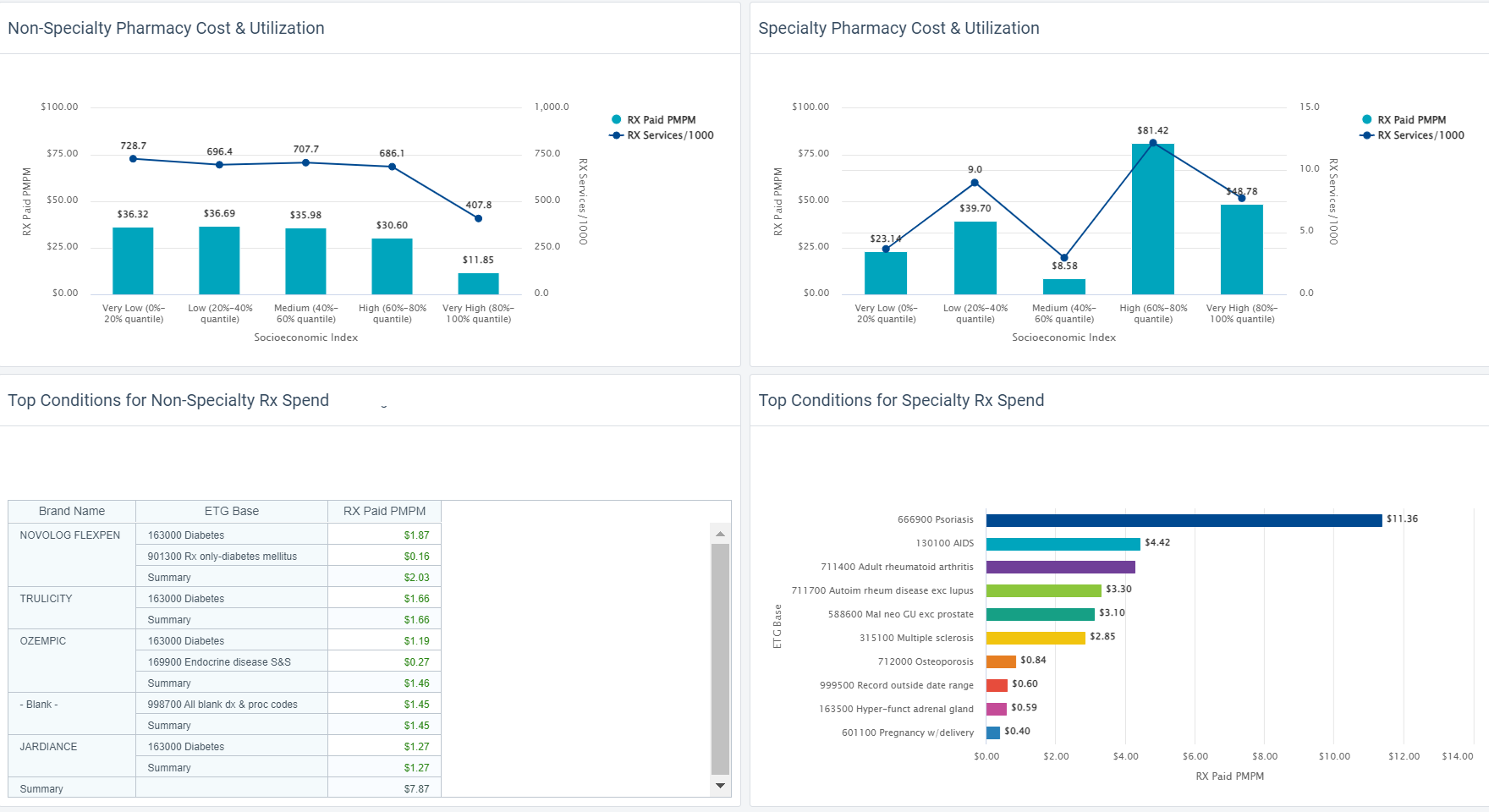
Measuring these differences allows us to take what we anecdotally see or suspect, and support it with facts.
Collegaues focused on Diversity, Equity, and Inclusion (DEI) agendas are wonderful partners. Share these insights with them. The numbers give your organization a brilliant set of facts to help drive decisions aligned to company goals.
We’ll help you surface these insights at your organization. Contact us to hear more about the possibilities.
With digital transformation improving health experiences, we now have even more Big Data in healthcare to use for deeper insights in population health.
When it comes to health analytics and DEI efforts, what data do you need? How do you get it? How can you get started? What happens next?
We’re so glad you asked – hear from our experts.
Originally presented as part of an AHIP webinar series.
Watch now Download the slides

through the lens of diversity equity, and inclusion.

Rani Aravamudhan is a more than a physician, specializing in General Medicine. She has extensive experience in the EMR/EHR and population-health industries with a focus on clinical transformation, workflow design and development, value-based care, risk management and clinical quality and performance reporting. Her strong background in clinical medicine and experience in the HIT industry make her successful in navigating payer, provider, and technology vendor landscapes.

Jason Elliott is Vice President of Customer Experience for Employer clients at HDMS. A true public health enthusiast with a Masters in Epidemiology, he spent over a decade delivering dedicated clinical analytics and leadership at BCBS. Since then, Jason has managed the managed the Employer practice area. He brings very structured thinking into the types of problems his clients are trying to solve, and what can be done with the insights discovered.
We have so many new reasons to use these advanced approaches to offset rising costs of care and challenging health conditions: deferred care, the increased need for mental health care, and virtual care adoption are disrupting historical patterns.
Learn how predictive analytics should fit into an overall analytic strategy. Invest in capabilities that allow you to act upon results, instead of sitting in reports in your inbox. Predictive analytics, when put to purpose, can be an instrumental part of a broader strategy to drive down costs and improve health.
Make sure you have the big picture so you get the most from these investments.
Originally presented as part of an AHIP webinar series.


Rani Aravamudhan is a more than a physician, specializing in General Medicine. She has extensive experience in the EMR/EHR and population-health industries with a focus on clinical transformation, workflow design and development, value-based care, risk management and clinical quality and performance reporting. Her strong background in clinical medicine and experience in the HIT industry make her successful in navigating payer, provider, and technology vendor landscapes.

Keith Wilton is the Vice President of Product Management, with more than 15 years’ experience in Product Management and an emphasis on creating and deploying complex software applications. Keith joined HDMS in March 2016 after serving as Vice President of Product Management at a leading player in the Alternative Investment space. Prior, Keith ran product management for an arm of Morgan Stanley, and for other organizations.
Hosted by Employee Benefit News & Employee Benefit Adviser
You’re doing all the right things – adhering to government and CDC safety measures, adopting state and local guidance into your operational policies and you’ve offered flu shots. What else should you be doing to keep your essential workers and their families healthy this winter and next year?

You are probably a bit overwhelmed, trying to ensure the safety of your employees and their contribution to smooth, reliable business operations, as winter approaches. With the convergence of COVID and flu season bringing new challenges, using your data in new and insightful ways becomes essential too. You can navigate the impact of emerging trends in virtual care, mental health, parental leaves and COVID-19 testing results. HDMS would like to give you some ideas about using analytics to quiet the chaos and make the best decisions for the care and costs of your most essential asset – your employees.
Join this webinar to connect 5 health care and benefits trends to analytic strategies that will best serve the health needs of your essential workforce this winter and beyond. HDMS, experts in health data, will share:
Leave with an understanding of how to create a streamlined strategy which uses analytics to monitor essential employee health and prepares you for decisions. Take away new ideas for metrics and leading indicators you can monitor to anticipate needs and budget more confidently!
Listen to how Meritain harnesses their powerful analytics to build strategic value with (and for) their clients. Meritain ensures new plan sponsor requirements and changing member behaviors inform innovation and planning.
With health care transforming right before our eyes, we need timely and quality data along with a means of turning on a dime more than ever before.
Watch now
Health insurance providers play an important role in helping plan sponsors navigate complex business decisions and necessary change during uncertainty and transformation. Data can be a beacon of light, giving us facts to shape where and how to best pivot. Data uncovers the areas we can be most helpful to plan sponsors and members.
Learn how to develop a strong framework with the right structures in place. Roll with new waves of regulations, coverage changes and payments or anything else that comes your way.
Attendees will learn:
New data analytics from HDMS uncovered some startling statistics about the impact of mental health conditions on the total cost of care. In the current environment, stress and anxiety are driving increased demand for mental and behavioral health services.
There is no one-size-fits-all solution, so using data to understand your population is crucial.

In this presentation, you will hear fresh data-driven approaches adopted by health insurance providers that will continue to create new industry standards in our changed world – from current telehealth engagement and utilization for mental and behavioral health conditions/substance abuse to reimbursement practices.
How do you support a member trying to manage their diabetes, obesity, and hypertension with the added anxiety post-pandemic?
Attendees will learn how to:
Speaker:
Robert Corrigan, Director of Advisory Services, HDMS

Speaker: Rani Aravamudhan, Senior Clinical Consultant, HDMS
